2 April 2020 (Brussels, Belgium) – Ah, hope springs eternal. Social distancing works. Excitement reigns. According to Sir Patrick Vallance, the UK Government’s Chief Scientific Officer, the London School of Hygiene and Tropical Medicine (LSHTM) estimated that before the lockdown one positive person with the coronavirus would infect 2.6 other people. Now it’s just 0.62. This means the virus is cornered – it has nowhere to go and will burn out. Good news.
Well, not quite. There is a raging battle across social media over “good data/bad data”. And inferred data and how we get “real” data. And how you establish a baseline. But let’s face it: there are a lot of figures involved in understanding the coronavirus pandemic, be it around cases, deaths or tests. But there is one number above all others that experts obsess on – the reproductive value, or “R0”.
First, some background
Speaking at the daily Downing Street press conference on Monday, Sir Patrick Vallance said “Britain’s lockdown is having a very big effect on the R0, bringing it down to below one”. But what does this actually mean and why does it matter? What is the R0 value?
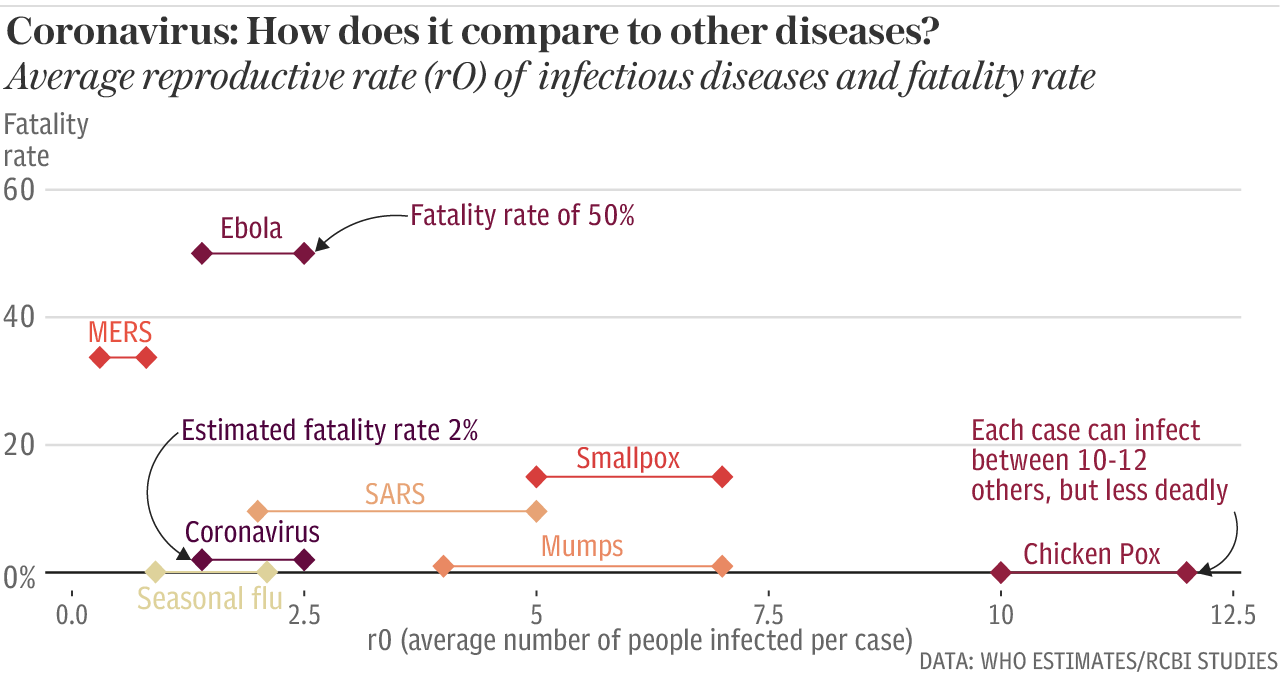
The reproductive value describes the average number of people an infected individual can expect to pass the coronavirus onto. It is therefore a measure of how transmissible, or contagious, a disease is. If a virus has an R0 of three, it means that every individual infected will pass the disease onto three other people if no containment measures are introduced. Jonathan Ball, professor of molecular virology at the University of Nottingham:
“The reason we’re interested is because it not only gives you an idea of how many people the virus is likely to infect, but also an idea about how effective your interventions need to be to end the outbreak.”
What is the reproductive rate for Covid-19? The World Health Organization estimated at the start of March that the coronavirus’ R0 stands somewhere between 2 and 2.5. By comparison seasonal flu is estimated to be roughly 1.3 while measles has a reproductive value of between 12 and 18. But these figures are not set in stone because the transmissibility of a disease is not based on biology alone. Professor Ball again:
“R0 is an indication of how much an infectious virus will spread in a population, and various things impact that value. The susceptibility, size and density of the population that the infection is introduced into matters, as well as the infectiousness of the virus itself.”
Estimates of the R0 for Covid-19 still vary, partly because we still do not know how many people have been infected in total. According to modelling published by Imperial College London this week, the R value stood somewhere between 3 and 4.6 in Europe before lockdowns came into effect. It’s also worth noting that the R0 is a measure of how infectious a disease is, but not how deadly.
What does Sir Patrick mean when he talks about the R0 value dropping below one? To bring an outbreak under control the R0 value needs to drop below one. This means that every infected individual passes the disease to less than one other person, causing the epidemic to die out. But as long as the number remains higher than one, the epidemic will grow.
Which interventions can help reduce the R0? There are lots of infection control measures experts can use to push this number down and “flatten the epidemiological curve”. As I noted earlier this week, a study in the Lancet, for instance, estimated that travel restrictions in Wuhan caused R0 to drop from 2.35 to 1.05 after just one week. Sir Patrick said that the stringent physical distancing measures introduced in the UK have had a substantial impact so far. As fewer people come into contact with one another, there are fewer opportunities for the virus to spread:
“We are seeing a dramatic reduction in transport being used and we know of course that things like restaurants and pubs where people aggregate. So we are seeing a big change on contacts. That is predicted to have a very big effect on the so-called R.”
According to a pre-print study from the London School of Hygiene and Tropical Medicine published this week and referenced by Sir Patrick, the average number of people an individual comes into contact with each day has dropped by 73 per cent since the UK’s lockdown began. From the study:
“This would be sufficient to reduce R0 from a value from 2.6 before the lockdown to 0.62 during the lockdown, indicating that physical distancing interventions are effective.”
“Just hold on there”, say critics of the study
The study tracked over 1,300 adults and has not yet been peer reviewed. But it is circulating amongst epidemiology experts and mathematicians, who find problems. For instance: how is LSHTM reaching its figures in absence of widespread testing? Is it based on confirmed cases?
The researchers agreed. It’s a reasonable question. The transmission figures rest on an estimate of the number or percentage of infected people in the general population. As this hasn’t been measured, it’s reasonable to ask how was it estimated. Does it mean we should assume the LSHTM numbers are wrong? No, but it’s reasonable to ask how they calculated.
And as one epidemiology expert opined, it will only burn out if we stay home indefinitely. In order to escape lockdown, the UK needs to develop mass testing and mass contact tracing solutions like they did in China and South Korea. Otherwise, we get a second wave and exponential growth. Granted: the UK and the US are finding mass testing to be hard, if not impossible, but there is no other way. Although France and Germany are doing it and they have shown us it limits contagion – so why has the UK government taken over 2 weeks to implement it?
And, of course, there are those that do not believe any of the projections by LSHTM. They say “How come the UK’s R0 is 0.62 on soft lock down when China only got 0.9 from a draconian lock down?”
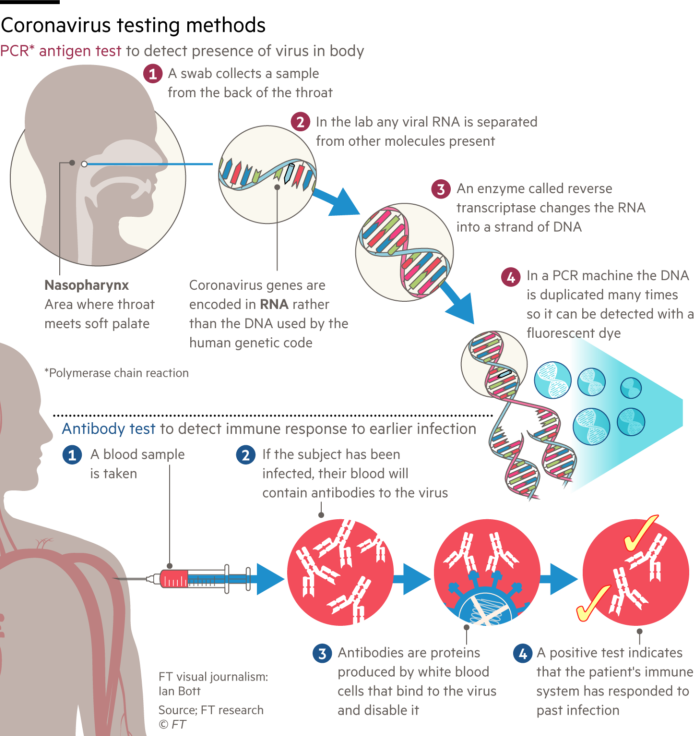
There is a bigger issue, too. We still need an antibody test. Most of the media still does not seem to appreciate the difference between the antibody test and the antigen test. Everybody is focusing on the latter when it is the former that will get us out of this. And without making this post too long, just a few more basics.
There are two main types of tests available for the coronavirus infection:
• The first, an antigen test, detects the presence or absence in the body of the new coronavirus, which causes the disease Covid-19.
• The second, an antibody test, looks for signs that someone has been infected in the past by searching for an immune response.
Since Chinese scientists in mid-January published the full genetic code of the virus, laboratories anywhere in the world have been able to use antigen testing to identify its genes in samples from patients. They use a procedure called polymerase chain reaction (PCR) that has been standard practice in labs for 30 years. PCR samples can come from several different sites in the patient. Simplest is the nasal swab taken from well inside the nose. The back of the throat is another option. For patients in hospital, a sample from the lower respiratory tract may give the best results. Antigen testing reveals whether someone has a current infection and could therefore pass Covid-19 on to others.
A graphic from the Financial Times to explain:
In contrast, antibody (or serological) tests work on blood samples to detect the immunity conferred by past infection. The test kits use proteins from the virus as “glue” to trap antibodies present in blood. To quote from the Financial Times:
A finger prick should provide enough blood to detect two types of antibodies against this coronavirus. The first, IgM antibodies, are shortlived and may indicate that the virus is still present. They usually disappear a couple of weeks after infection.
In their place emerge a second more durable type, IgG antibodies. No one knows yet how long these will last and provide resistance to reinfection — anything from a few months to a few years seems possible.
Antibody tests are being prioritised by governments including the UK and Germany because they will be essential to informing individuals whether they can return to mixing safely in society without passing on or picking up infection. When carried out in a representative sample of the population, they will also answer key epidemiological questions — including about how many people were infected with mild or no symptoms. Once developed, antibody tests should give results more quickly than traditional PCR tests, taking a few minutes rather than a few hours, though much faster antigen kits are under development.
So you probably see the problem. When health authorities began to realise that the coronavirus outbreak might pose a global threat, they started developing tests in government labs such as those operated by U.S. Centers for Disease Control and Prevention and Public Health England, which already had ample experience in using PCR technology for diagnostics.Traditionally, antigen diagnosis is done mostly in the public sector, with private companies providing test components such as chemical reagents and swabs for patient samples – some of which have been in short supply.
But these are conventional labs, not equipped for a massive ramp up. Governments realized they needed a huge mobilisation of private sector resources (who have the capacity) because they can roll out automated PCR kits that process samples much more quickly than conventional labs. This partially explains the disconnects and timing delays in both the U.S. and the UK.
But not in Germany which outclassed them on response and really needs a separate post to explain all the things they did right. In brief: German public health officials and independent study by the Johns Hopkins University Coronavirus Center in the U.S. (the Johns Hopkins Department of Epidemiology is the oldest, and among the largest, in the world) have estimated that German laboratories are carrying out as many as 500,000 coronavirus tests a week. Though “official” data has yet to confirm that number, it suggests that testing capacity has expanded fast in recent weeks. Germany’s decentralised and extensive test and laboratory infrastructure means the work is carried out not just in hospitals and doctors’ practices but also in special drive-in stations.
And two key points, repeated in much of the scientific literature:
*New antigen tests are relatively easy to create because the PCR test is a small addition to an existing test.
*But antibody tests take longer to develop because they have to be created from scratch. You need to physically get patient blood, find the antibodies in that blood (molecules smaller than the virus), create a reproducible antibody in the lab, and then create a reagent test that will react in the presence of that antibody.
Oops. I digressed. Three last points:
• The significance of the LSHTM estimation is that the virus can be controlled by using very severe measures. The key question is whether the transmission factor can be kept comfortably below 1 just by using “sensible precautions”. And it is going to be a long while before we get a vaccine. I do not see things going back to “normal” any time soon.
• As to the LSHTM numbers, it’s an inferred figure with a poor degree of confidence on the estimate. If we have 1,000 cases and a high R value of say 5, that means 5,000 new cases. But if we have 100,000 cases and an R value of just 0.5, we still get 50,000 new cases. We need to see what real, extensive testing does. We need a “real” baseline.
Because one of the challenges that has made the pandemic so difficult to control is that research increasingly suggests a large number of people infected with the virus may show no symptoms — as many as 25 percent, according to U.S. officials and 35% according to UK officials. That means that in places with limited testing, doctors and scientists know they are missing people who are infected with the virus — and may be spreading it to others.
• And the virus won’t burn out “just like that” as many say. Even measles has not completely burned out. The disease will burn out to a significant level but it will take several cycles. Antibody tests, if reliable, will help.